- Visibility 344 Views
- Downloads 38 Downloads
- Permissions
- DOI 10.18231/j.ijpo.2022.064
-
CrossMark
- Citation
Adenoma malignum of cervix – A case report
- Author Details:
-
Srinidhi R *
-
Veena Ramaswamy
-
Tejaswini B N
-
Sowmya B U
Abstract
Adenoma malignum also called minimal deviation adenocarcinoma or minimal deviation carcinoma, is a rare disease. It is tricky to diagnose this condition because of its benign look. It forms a subtype of mucinous endocervical adenocarcinoma. Also, these lesions have an endophytic growth and are located deep in the cervix rather than an exophytic growth like any other adenocarcinoma of the cervix. Radiologically and clinically can resemble a benign, less harmful disease. However, it sometimes mimics multiple Nabothian cysts because of its benign look. In most cases, it had been an incidental finding when being evaluated for any other causes where hysterectomy was done. It usually presents between the age of 25-70 years and peaks at a median age of 42 years. Thus, this case report is an eye opener to keep Adenoma malignum is a close differential for watery discharge per vaginum. Although it is a rare tumour, it has an aggressive nature.
Introduction
Adenoma malignum was first discovered by Gusserow as a highly differentiated adenocarcinoma of the cervix in 1870. The word adenoma indicates the benign appearance of the cells, and malignum is for virulent progression of the disease. It is also called Minimal deviation adenocarcinoma or gastric type adenocarcinoma. It forms 1-3% of the endocervical adenocarcinoma.[1] At times, it mimics multiple Nabothian cysts because of its benign look.[2], [3], [4] It usually presents between the age of 25 to 70 years and peaks at a median age of 42 years.[5]
Case Report
A 35-year aged female presented with complaints of post-coital bleeding and watery discharge per vaginum. On examination of the abdomen, no significant findings. Bilateral inguinal lymph nodes were palpable. The bilateral breast showed no lumps. Per speculum, 2cm raw congested area on the posterior lip of cervix that bleeds on touch. Her liquid-based cytology PAP smear showed atypical glandular cells. The patient underwent an MRI pelvis 2.6x1.7x2.4cm hyperintense heterogeneously enhancing mass involving the cervix with cervical stromal invasion. Prominent bilateral external ilial lymph nodes are also seen.

Hysteroscopy showed fluffy, fragile growth and biopsy were done from the lesion. Microscopy showed Papillaroid endocervical epithelium lined by columnar cells with stratification and pleomorphism.

She underwent radical hysterectomy with bilateral salpingectomy and bilateral ovarian transposition with lymph node dissection.
Grossly a homogenous grey white lesion was found to involve all four quadrants of the cervix, with the majority in the posterior quadrant measuring 2x1.4cm and the depth of invasion was 8mm. The rest of the uterine cavity, isthmus, bilateral ovaries, and fallopian tubes were unremarkable.
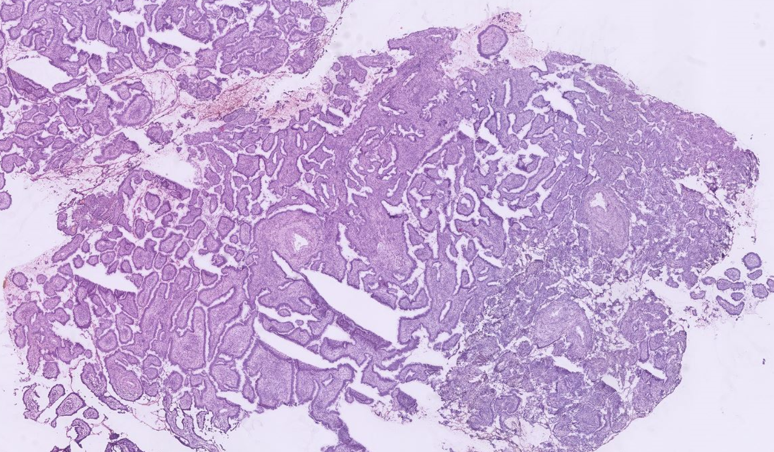
Microscopy of the resected specimen showed a similar appearance as the biopsy and was given as Adenoma malignum or minimal deviation adenocarcinoma. The margins and the regional lymph nodes were free of tumour. ([Figure 2])

The patient was given brachytherapy with external beam radiotherapy and is on follow up.
Discussion
Adenoma malignum is a type of mucinous adenocarcinoma of the cervix. The clinical presentation ranges from asymptomatic to vaginal bleeding or discharge.[1] The other clinical features include menorrhagia, mucoid discharge per vaginum, post-coital bleeding and post-menopausal bleeding, and rarely abdominal swelling.[5] Its pathophysiology is unclear, and some of these cases show atypical lobular atypical gland hyperplasia. It is associated with Peutz–Jeghers syndrome or hereditary intestinal polyposis (germline STK11 mutation), ERBB2 (HER2) and MDM2 amplification.[6] Few cases may not have any lesion grossly. Adenoma malignum can be an incidental finding when hysterectomy is done for any other cause.[7] Imaging can show a multicystic lesion with solid areas in the deep vaginal stroma whenever a lesion is present. Gadolinium enhancement can help identify solid areas.[8] The microscopic features include large sheets of cells with honey comb pattern palisading and abnormal glandular cells in the periphery with abundant mucin. There will be well spaced, deeply invasive branching glands with intraluminal papillary projections. The stroma will be edematous and show desmoplasia.[1] Although there is no standard protocol to diagnose adenoma malignum, the initial investigations should include hysteroscopy, ultrasound, MRI pelvis, and biopsy for histopathology correlation.[9] It is an aggressive chemorefractory tumour with possible peritoneal and abdominal spread. Most of them are diagnosed at an advanced stage. The prognosis is worse than any other type of adenocarcinoma cervix.[1]
Conclusion
Adenoma malignum is a rare tumour, and there is no established screening tool for evaluation. It can be misdiagnosed as benign. It is an aggressive tumour and should be kept in mind while evaluating cases of post-coital bleeding or discharge per vaginum.
Source of Funding
None.
Conflict of Interest
None.
References
- Ki E, Byun S, Park J, Lee S, Hur S. Adenoma malignum of the uterine cervix: report of four cases. World J Surg Oncol. 2013;11(1):1-6. [Google Scholar]
- Lim K, Lee I, Kim T, Kwon Y, Jeong J, Shin S. Adenoma malignum of the uterine cervix: Clinicopathologic analysis of 18 cases. Kaohsiung J Med Sci. 2012;28(3):161-4. [Google Scholar]
- Yamashita Y. Adenoma malignum: MR appearances mimicking nabothian cysts. AJR. 1994;162:649-50. [Google Scholar]
- Chang J, Zhang S, Zhou H, Liang J, Lin Z. Clinical analysis of minimal deviation adenocarcinoma of the cervix: a report of five cases. Ai Zheng. 2008;27(12):1310-4. [Google Scholar]
- Weerakkody Y, El-Feky M. Adenoma malignum of the cervix. . . [Google Scholar] [Crossref]
- Gilks C, Young R, Aguirre P, Delellis R, Scully R. Adenoma malignum (minimal deviation adenocarcinoma) of the uterine cervix. A clinicopathological and immunohistochemical analysis of 26 cases. Am J Surg Pathol. 1989;13(9):717-29. [Google Scholar]
- Kamath G, Bhatt A, Ramaswamy V. A rare case of adenoma malignum: preparing for the unforeseen. J Obstet Gynecol India. 2017;67(1):70-3. [Google Scholar]
- Okamoto Y, Tanaka Y, Nishida M, Tsunoda H, Yoshikawa H, Itai Y. MR imaging of the uterine cervix: imaging-pathologic correlation. Radiographics. 2003;23(2):425-45. [Google Scholar]
- Mills K, Shuen P, Zolis L. Adenoma malignum presenting with profound hyponatremia. J Obstet Gynaecol Can. 2015;37(7):624-7. [Google Scholar]
How to Cite This Article
Vancouver
R S, Ramaswamy V, N TB, U SB. Adenoma malignum of cervix – A case report [Internet]. Indian J Pathol Oncol. 2022 [cited 2025 Oct 25];9(3):274-276. Available from: https://doi.org/10.18231/j.ijpo.2022.064
APA
R, S., Ramaswamy, V., N, T. B., U, S. B. (2022). Adenoma malignum of cervix – A case report. Indian J Pathol Oncol, 9(3), 274-276. https://doi.org/10.18231/j.ijpo.2022.064
MLA
R, Srinidhi, Ramaswamy, Veena, N, Tejaswini B, U, Sowmya B. "Adenoma malignum of cervix – A case report." Indian J Pathol Oncol, vol. 9, no. 3, 2022, pp. 274-276. https://doi.org/10.18231/j.ijpo.2022.064
Chicago
R, S., Ramaswamy, V., N, T. B., U, S. B.. "Adenoma malignum of cervix – A case report." Indian J Pathol Oncol 9, no. 3 (2022): 274-276. https://doi.org/10.18231/j.ijpo.2022.064
