- Received November 30, -0001
- Accepted November 30, -0001
- Publication March 08, 2021
- Visibility 10 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijpo.2020.040
-
CrossMark
- Citation
A 2 year study of clinico-hematological profile of bicytopenia and pancytopenia in paediatric patients attending a tertiary hospital in South India
- Author Details:
-
Renu Thambi
-
Ginju Vijayakrishnan *
-
Sankar S
Introduction
Pancytopenia refers to a decrease in all the three cell lines of blood viz. RBCs, WBCs and Platelets, while bicytopenia refers to reduction in any two out of the three. Pancytopenia is diagnosed when the hemoglobin (Hb) <10g%, absolute neutrophil count (ANC) <1.5 x 109/L and platelet count <100 x 109/L. It is labelled severe if patient has two or more of the following: Hb <7 gm%, ANC <0.5 x 109/L, and platelet count <20 x 109/L.[1] Pancytopenia has a wide etiological profile, ranging from simple drug-induced bone marrow hypoplasia, nutritional deficiencies to fatal bone marrow aplasia and leukemia. Identification of correct cause is mandatory as it will help in implementing appropriate therapy and assessing the prognosis.[2] Etiological classification of pancytopenia can be done into three groups- failure of production (implying intrinsic bone marrow disease), sequestration (hypersplenism), and increased peripheral destruction.[3]
Failure of bone marrow can be due to primary production defects. Primary or genetic causes include Fanconi anemia, dyskeratosis congenita, Shwachman-Diamond syndrome, and amegakaryocytic thrombocytopenia.[4] The production of hemopoietic cell can also be prejudiced in the bone marrow either by infections, toxins, and malignant cell infiltration leading to hypocellular marrow.[5]
When pancytopenia is associated with organomegaly and lymphadenopathy, the possibility of malignancies or bone marrow failure syndromes are considered. There are a number of other causes which can present in the similar way.[6]
Acquired causes of pancytopenia can be nutritional deficiencies, idiopathic or secondary to exposure to radiation, drugs and chemicals (chemotherapy, chloramphenicol, sulfa drugs, antiepileptics, gold etc), viral infections (cytomegalovirus, Epstein-Barr virus, hepatitis B or C, HIV etc.), auto-immune, paroxysmal nocturnal hemoglobinuria, and marrow replacement disorders (leukemia, myelodysplasia, myelofibrosis).[7] Megaloblastic anemia and infections such as enteric fever, malaria, kala-azar and bacterial infections are the common causes of pancytopenia in developing countries.[8]
Hypersplenism causes pancytopenia by splenic sequestration and in some cases by hemolysis.[9] The common causes of hypersplenism include cirrhosis, congestive heart failure, and malignancies like leukemia/lymphoma, hemoglobinopathies and infections.
Autoimmune-mediated disorders like systemic lupus erythematosis (SLE) can present with pancytopenia when all the three cell lines are affected. Patients with autoimmune disorders like rheumatoid arthritis, psoriasis and SLE are at increased risk for lymphoproliferative disorders and it is important to exclude underlying malignancies like lymphoma while evaluating these patients.[10], [11], [12] Autoimmune cytopenias are also seen in autoimmune lymphoproliferative syndrome (ALPS) and common variable immunodeficiency disease (CVID).
Paroxysmal nocturnal hemoglobinuria and hemophagocytic lymphohistiocytosis can cause both impaired production and increased peripheral destruction of blood cells.
The aim of this study is to describe the different aetiologies of bicytopenia and pancytopenia in paediatric patients based on clinical and haematological profiles including peripheral blood and bone marrow examination.
Materials and Methods
This descriptive study was undertaken for a period of 6 months (analysis of cases from January 2015-December 2016) at a tertiary care center in central Kerala. All cases of paediatric pancytopenia and bicytopenia with age <12 years based on complete blood count and admitted in the institute during 2 year period from January 2015-December 2016 were taken for the study. Patients beyond these age limits, previously diagnosed cases of aplastic anaemia and leukemia, cases with clinical suspicion of genetic or constitutional pancytopenia, patients with history of blood transfusion in the recent past, and those who were not willing for admission were excluded.
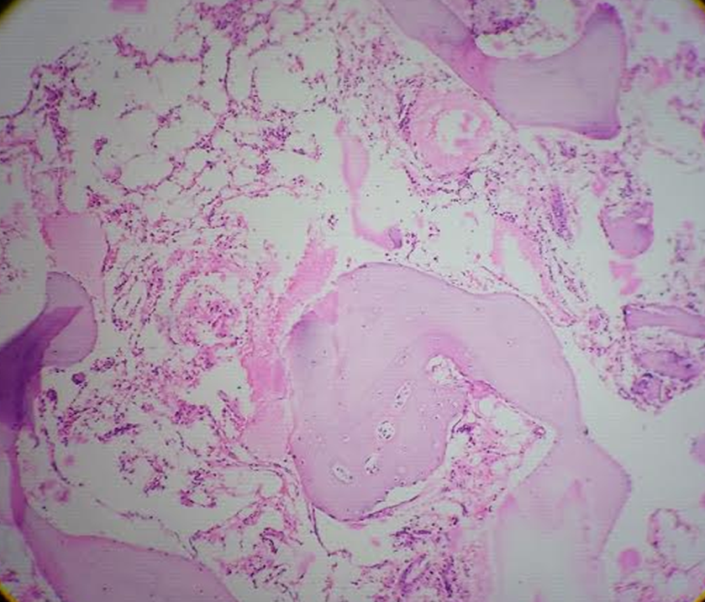
A systematic review of clinical findings provided in the request forms submitted in the lab was done. Complete blood counts(CBC), peripheral smear and bone marrow findings in each case were recorded. Hematological profile(CBC) included hemoglobin, red cell indices, total and differential leukocyte counts, platelet count, peripheral blood smear morphology and bone marrow aspiration/biopsy. Blood counts were done on automated hematology analyzer (sysmex). Platelet counts obtained from counter were confirmed by peripheral blood smear examination. Bone marrow aspiration and trephine biopsy stained with Leishman and hematoxylin and eosin stain respectively, along with special stains were reviewed in cases where they were done. Cytopenia was defined as: hemoglobin < 10g/dL, total leukocyte count < 4 × 109/L and platelet count < 100 × 109/L and adjustments for age were made wherever necessary. Follow up of patients with CBC and peripheral smear was attempted. The data was entered in Microsoft excel and further statistical analysis was done using IBM SPSS software statistics 20 trial version.
Results
Age group most commonly affected in our study was 9-12 years. Cytopenia affected females more than males (M:F-0.9:1). Most of the children presented with fever and the most common clinical findings were fever, pallor and organomegaly. Hepatomegaly was the most commonly elicited sign ([Table 1]).
Infections were found to be the major cause of bi/pancytopenia in children who needed hospital admission ([Table 2]). Dengue fever constituting 34% of the cases was the most common type of infection requiring inpatient care. Second most common cause of bi/pancytopenia was acute leukemia followed by aplastic anemia. No specific identifiable causes were noted in 10 out of 117 cases.
In our study, Bicytopenia cases outnumbered Pancytopenia cases (82 cases vs 35cases). Among bicytopenia cases, combination of anemia and thrombocytopenia was seen in maximum cases followed by anemia and leukopenia. Acute leukemia presented as either bicytopenia or pancytopenia in 30 cases of which majority were bicytopenia (70%).
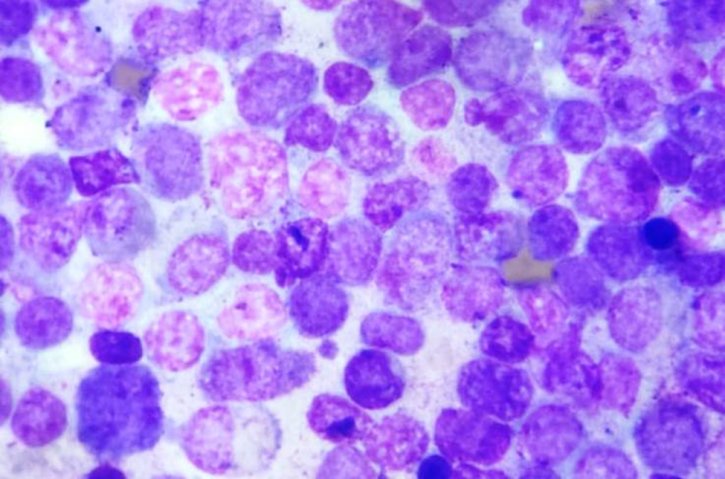
Bone marrow study was done in 63 out of 117 cases, out of which acute leukemia (25.8%) was the most common diagnosis. Acute lymphoblastic leukemia constituted the maximum number (22.2%) of cases among acute leukemia ([Figure 1]).

| Signs and Symptoms | Frequency | Percent |
| Fever | 79 | 67.52 |
| Pallor | 25 | 21.37 |
| Bleeding | 11 | 9.40 |
| Jaundice | 4 | 3.42 |
| Bone pain | 6 | 5.13 |
| Hepatomegaly | 33 | 28.21 |
| Splenomegaly | 25 | 21.37 |
| Testicular enlargement | 1 | 0.85 |
| Lymph node enlargement | 21 | 17.95 |
| Cause of bi/pancytopenia | Frequency | Percent |
| Infection | 56 | 47.86 |
| ALL | 26 | 22.22 |
| AML | 4 | 3.42 |
| ITP | 6 | 5.13 |
| Hereditary Spherocytosis | 1 | 0.85 |
| Megaloblastic anemia | 3 | 2.56 |
| Aplastic anemia | 6 | 5.13 |
| Immune hemolytic anemia | 2 | 1.71 |
| Lysosomal storage disease | 1 | 0.85 |
| Diamond Blackfan syndrome | 2 | 1.71 |
| Non contributory | 10 | 8.5 |
| Total | 117 | 100.0 |
Discussion
Age group most affected in our study was >9 years. Different studies showed marked variation in the age groups affected which emphasized the lack of correlation between age affected and cytopenia.
Females were affected by cytopenia more than males in our study (0.9:1) which was comparable with the study done by Dubey S et al (0.88:1).[13] Many studies showed male predominance, which may be due to variations in the inclusion criteria applied.
Most common presenting symptom was fever (67.52%) which was comparable with studies done by Dubey S et al(68%),[13] Rathod GB et al(65%),[14] Jan A et al(62.85%),[15] Memon S et al(65%)[16] and Khan FS et al(68%).[17] Hepatomegaly was the most commonly elicited sign(28.21%), similar to the study by Sharif M et al with hepatomegaly seen in 27.6% of cases[18] ([Table 3]).
Most common bicytopenia seen in our study was anemia and thrombocytopenia, with similar findings reported in studies by Dosi S et al[19] and Varma N et al[20] ([Table 3]). Bicytopenia could be due to significant marrow disease as in cases of acute leukaemia or due to 2 different pathological processes occurring together. Therefore it is essential to differentiate between the two and identify those cases which need urgent investigations and treatment. In our study, bicytopenia due to anaemia and thrombocytopenia was coexisting nutritional deficiency and viral infections.
The proportion of acute leukemia in bicytopenia and pancytopenia in our study was comparable with the studies by Dosi S et al[19] and Waris R et al.[21]
We observed that the most common cause of cytopenia in our study was infections followed by acute leukemia and aplastic anemia. Most of the studies showed the common causes as megaloblastic anemia and aplastic anemia followed by acute leukemia. This difference could be due to the fact that we included only hospitalized patients with cytopenia. In addition to marrow diseases, those severe infections like dengue fever (34%) warranted hospital stay and hence was included in our study.
| Thambi R et al (2019) | Dosi S et al (2018)19 | Waris R et al(2017)21 | Dubey S et al (2016)13 | Rathod GB et al (2015)14 | Sharif M et al (2014)18 | Jan A et al (2013)15 | Varma N et al (2011)20 | Memon S et al (2008)16 | |
| Study period | 2 years | 5 years | 15 months | 18 months | 1 year | 1 year | 6 years | 2 years | 18 months |
| Sample size | 117 | 107 | 154 | 170 | 200 | 105 | 205 | 571 | 230 |
| Bicytopenia | 82 | 48 | 85 | - | - | 66 | - | 396 | - |
| Pancytopenia | 35 | 59 | 69 | 170 | 200 | 39 | 205 | 175 | 230 |
| Age range | 0-12 years | 2 months - 16 years | 2 months - 12 years | 1- 18 years | 6months-14years | 2 months-12years | 6 months-14years | 0-12 years | 2 months-15years |
| Most common bicytopenia combination | Anemia + thrombocytopenia | Anemia + thrombocytopenia | - | - | - | - | - | Anemia+Thrombocytopenia | - |
| Common cause | Infection> Acute Leukemia > Aplastic Anemia | Bicytopenia-Acute lymphoblastic leukemia > megaloblastic anemia > iron deficiency anemia. Pancytopenia-megaloblastic anemia > acute lymphoblastic leukemia > aplastic anemia | Bicytopenia-Acute leukemia > Enteric fever > megaloblastic anemia. Pancytopenia-Aplastic anemia > acute leukemia > megaloblastic anemia | Megaloblastic anemia > Aplastic anemia > Acute leukemia | Megaloblastic anemia > Aplastic anemia > Acute leukemia | Megaloblastic anemia > Infective etiology > Aplastic anemia | Aplastic anemia > haematological malignancies > megaloblastic anemia | Bicytopenia-acute Leukemia > Non-specific causes > ITP Pancytopenia- Aplastic anemia > Megaloblastic anemia > Visceral leishmaniasis | Aplastic anemia > Megaloblastic anemia > Acute lymphoblastic leukemia,mixed nutritional anemia |
| Proportion of acute leukemia in bicytopenia | 21/82 | 13/48 | 23/85 | - | - | - | - | 241/347 | - |
| Proportion of acute leukemia in pancytopenia | 9/35 | 11/59 | 15/63 | - | - | - | - | 37/149 | - |
Limitations of the Study
Infections prevalent at the particular time of season requiring hospital admissions might have contributed more number of cases leading to a bias in the study.
Conclusion
Bicytopenia and pancytopenia in children indicates significant underlying pathology and in our study the most common aetiologies were infections, followed by acute leukemia and aplastic anaemia. Bi/pancytopenia presenting with fever, pallor and bleeding with organomegaly signify underlying bone marrow disorders /malignancies which warrants thorough work up. Peripheral smear and bone marrow examination help in diagnosing such cases.
Financial Support and Sponsorship
State board of medical research.
Conflicts of Interest
There are no conflicts of interest.
References
- F Frank, C Collin, P David, R Byran. . De Gruchey’s clinical hematology in medical practice. 5th ed 2004. [Google Scholar]
- B N Gayathri, Kadam Satyanarayan Rao. Pancytopenia: A Clinico Hematological Study. J Lab Physicians 2011. [Google Scholar]
- R Sharma, G Nalepa. Evaluation and Management of Chronic Pancytopenia. Pediatr Rev 2016. [Google Scholar]
- Robert A Brodsky, Richard J Jones. Aplastic anaemia. Lancet 2005. [Google Scholar]
- M Kar, A Ghosh. Pancytopenia. J Indian Acad Clin Med 2002. [Google Scholar]
- R Chand, N Singh. Clinico-etiological profile of pancytopenia in children: a tertiary care center based study of Kumaun region. Int J Contemp Pediatr 2018. [Google Scholar]
- Blanche P Alter. Bone marrow failure syndromes in children. Pediatr Clin North Am 2002. [Google Scholar]
- Shishir Kumar Bhatnagar, Jagdish Chandra, Shashi Narayan, Sunita Sharma, Varinder Singh, Ashok Kumar Dutta. Pancytopenia in Children: Etiological Profile. J Trop Pediatr 2005. [Google Scholar]
- J H Jandl, R H Aster. Increased splenic pooling and the pathogenesis of hypersplenism. Am J Med Sci 1967. [Google Scholar]
- Eva Baecklund, Anastasia Iliadou, Johan Askling, Anders Ekbom, Carin Backlin, Fredrik Granath. Association of chronic inflammation, not its treatment, with increased lymphoma risk in rheumatoid arthritis. Arthritis Rheum 2006. [Google Scholar]
- D Margolis, W Bilker, S Hennessy, C Vittorio, J Santanna, B L Strom. The risk of malignancy associated with psoriasis. Arch Dermatol 2001. [Google Scholar]
- E Zintzaras, M Voulgarelis, H M Moutsopoulos. The risk of lymphoma development in autoimmune diseases: a meta-analysis. Arch Intern Med 2005. [Google Scholar]
- Shiv Dubey, Saurabh Patel, A K Arya, R P Singh. Clinico-etiological spectrum of pancytopenia in hospitalized children. Int J Contemp Pediatr 2016. [Google Scholar]
- G B Rathod, M Alwani, H Patel, A Jain. Clinico-hematological analysis of Pancytopenia in Pediatric patients of tertiary care hospital. IAIM 2015. [Google Scholar]
- Anwar Zeb Jan, Bakhtyar Zahid, Samreen Ahmad, Zahid Gul. Pancytopenia in children: A 6-year spectrum of patients admitted to Pediatric Department of Rehman Medical Institute, Peshawar. Pak J Med Sci 2013. [Google Scholar]
- S Memon, S Shaikh, Maa Nizamani. Etiological spectrum of pancytopenia based on bone marrow examination in children. J Coll Physicians Surg Pak 2008. [Google Scholar]
- F Shafi Khan, R Fayyaz Hasan. Bone marrow examination of pancytopenic children. J Pak Med Assoc 2012. [Google Scholar]
- M Sharif, N Masood, Zahoor Ul Haq, Ahsan Dodhy, Muhammad Asghar. Etiological Spectrum of Pancytopenia/Bicytopenia in children 2 months to 12 years of age. J Rawalpindi Med Coll (JRMC) 2014. [Google Scholar]
- S Dosi, G Malpani, A Varma, K Malukani, P Kiyawat Jain, A Ajmera. Clinicopathological and etiological spectrum of bicytopenia/pancytopenia in children : A five year experience in a tertiary health care centre. Indian J Basic Appl Med Res 2018. [Google Scholar]
- Neelam Varma, Shano Naseem, Reena Das, Jasmina Ahluwalia, ManUpdesh Singh Sachdeva, RamKumar Marwaha. Pediatric patients with bicytopenia/pancytopenia: Review of etiologies and clinico-hematological profile at a tertiary center. Indian J Pathol Microbiol 2011. [Google Scholar]
- R Waris, G Shahid, S T Khalid, A Riaz, A Rehman. Aetiology of Cytopenias in Children Admitted to a Tertiary Care Hospital. JIMDC 2017. [Google Scholar]
